Managing Hospital Emergency Rooms
IMSI - September 2023
Managing Hospital Emergency Rooms
IMSI September 2023
The Institute for Mathematical and Statistical Innovation held a long program on, Mathematics, Statistics, and Innovation in Medical and Health Care which ran from March 27 to June 2, 2023.
The quantification of medical and health care has revolutionized human lives, with strong and long-lasting positive social and economic impact. This revolution stems from synergies among mathematics, statistics, data science, medicine, and machine learning (ML) and artificial intelligence (AI) which has prompted the creation of interdisciplinary areas across the various fields. Despite major progress in many scientific directions, there is a continuing need to develop existing areas and set the foundations for new ones. This need has been amplified by emergent events such as the recent COVID-19 pandemic. For example, the pandemic catalyzed cross-disciplinary work on patient flow through hospital emergency departments (EDs) among statisticians, operations researchers, actuaries, and AI/ML researchers. COVID was transformative in how hospitals organize the flow of patients during an unexpected extended emergencies which put stresses on limited resources such as beds in various departments, supplies, and staffing.
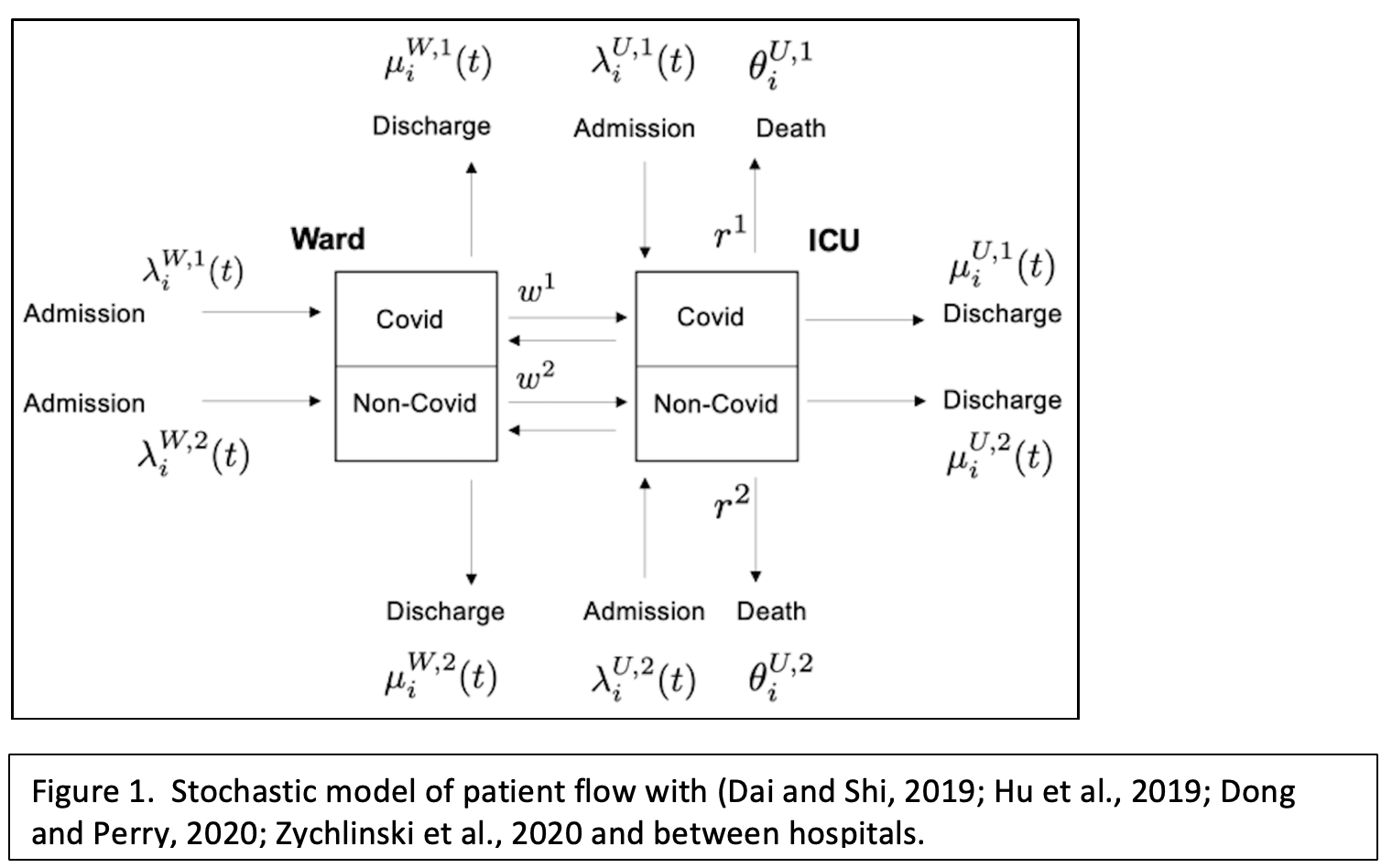
Vahid Sarhangian, a statistician at the University of Toronto who spoke at the program workshop on Predictive Analytics, Business Modeling and Optimization in Healthcare Operations Management, examined the admission, flow, and treatment of COVID vs. non-COVID patients. He recognized that there was a geographic mismatch between demand for hospitalization and hospital capacity during COVID pandemic. He described how high hospital occupancy is statistically associated with worsened health outcomes and higher mortality, and that there are associated equity issues around these facts. Sarhangian has developed a stochastic control model for flowing patients in and among hospitals that takes into account distances between hospitals and the costs of transferring patients (see Figure 1). He has proposed a solution for “load balancing” via inter-hospital transfers and has tested his model on 3000 transfers among hospitals in Ontario, Canada.
Hospital emergency departments are all too familiar to most of us, and the takeaway impressions for many are the crowds and long wait times coupled to high uncertainty about how long one will have to wait. The problem of predicting wait times is extremely complex because it depends on the number of patients in the ED at a given time, which is constantly changing, and triage such that a person’s place in line change based on the arrival of a patient in more urgent condition. Georgia Perakis, a professor of management at MIT who specializes in machine learning (ML) and operations research, discussed her work on using ML to manage triage in a data-driven way that is also equitable and fair during the program workshop on Analytics for Improved Healthcare. Complicating factors are that women tend to have longer wait times but not longer time to discharge, which could negatively impact health outcomes. Perakis hopes that her work will make the management of EDs more efficient for hospitals while improving health outcomes and the overall experience for patients.
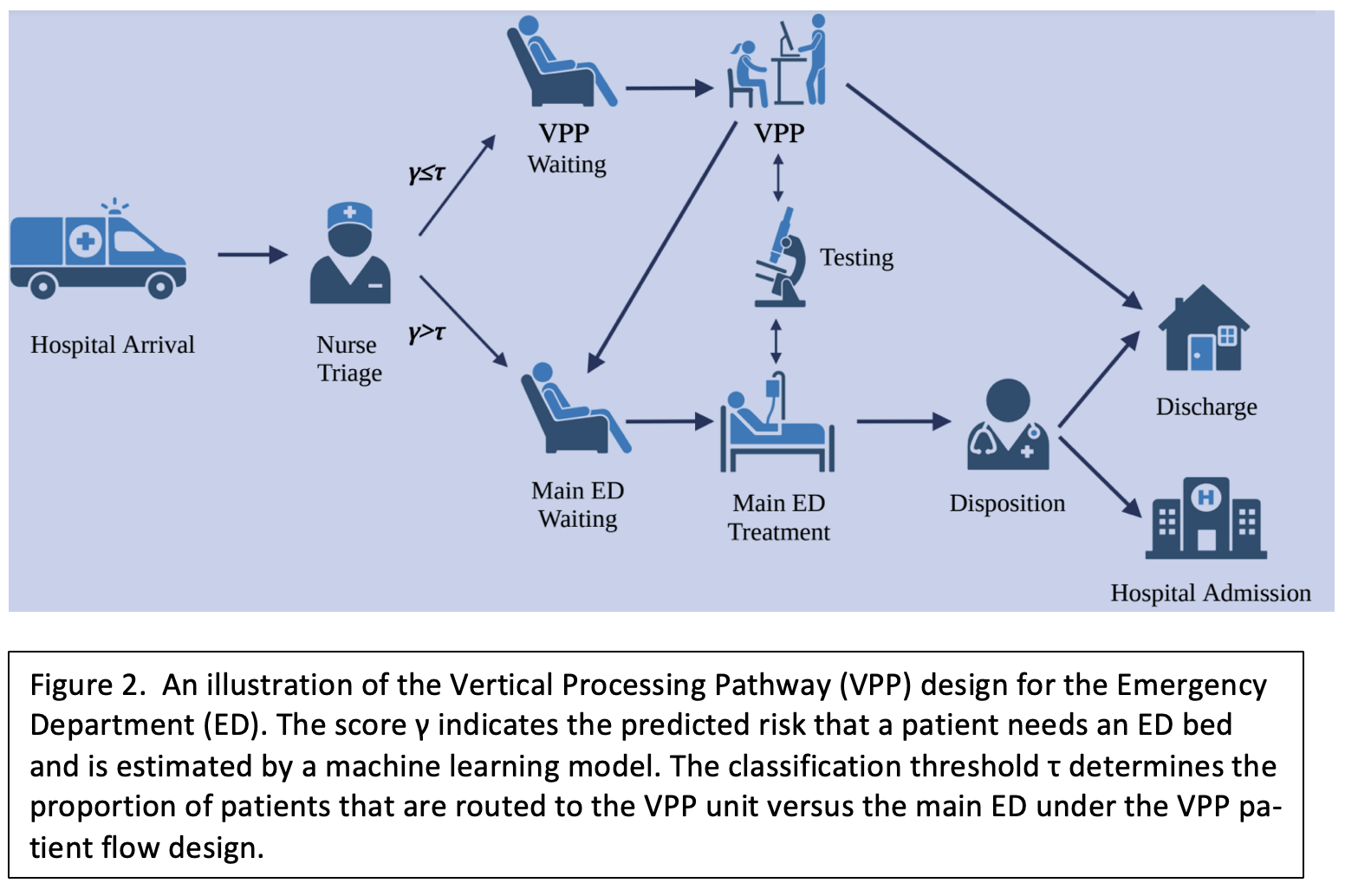
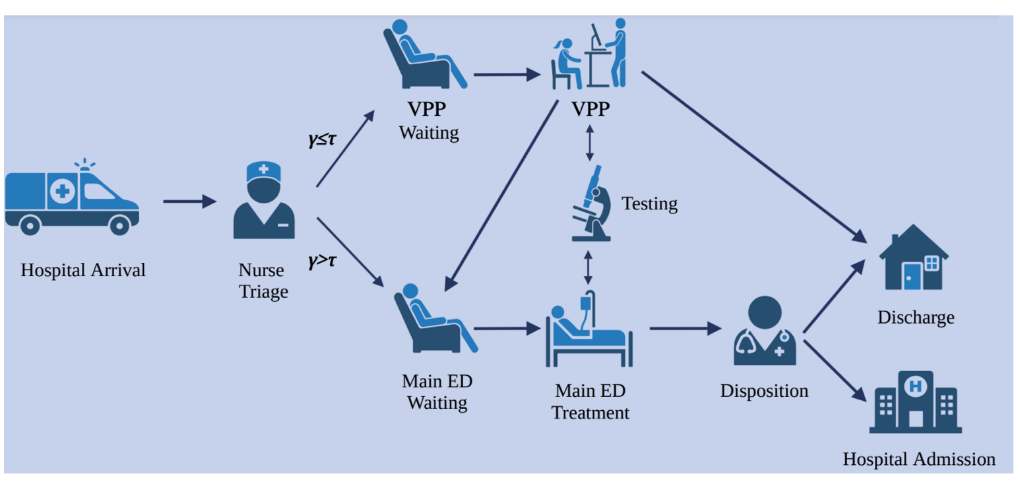
As noted above ED overcrowding is a major problem, not only during pandemics, which can lead to undesirable health outcomes such as abandonment (the patient leaves before being treated), the patient’s condition worsens while they are waiting, or patients are triaged inequitably. Agni Orfanoudaki, a professor of operations management at the University of Oxford and speaker in the Analytics for Improved Health Care workshop (also a program organizer), uses machine learning to improve operational efficiency in the ED, with a particular focus on nurse-driven “rapid medical assessment” (RMA). RMA is a strategy to triage patients nearly upon arrival to determine whether they need an ED bed or whether they can be treated more quickly while sitting up in a chair (see Figure 2). The goal should be to discharge as soon as possible everyone who receives an RMA and does not need an ED bed. Orfanoudaki is using training data in her ML model to make better predictions about which patients should be prioritized for a bed in the ED, versus those with relatively minor complaints who can be quickly treated and discharged.